First-of-its-kind patient experience EHR integration
First-of-its-kind patient experience EHR integration
How it works
How it works
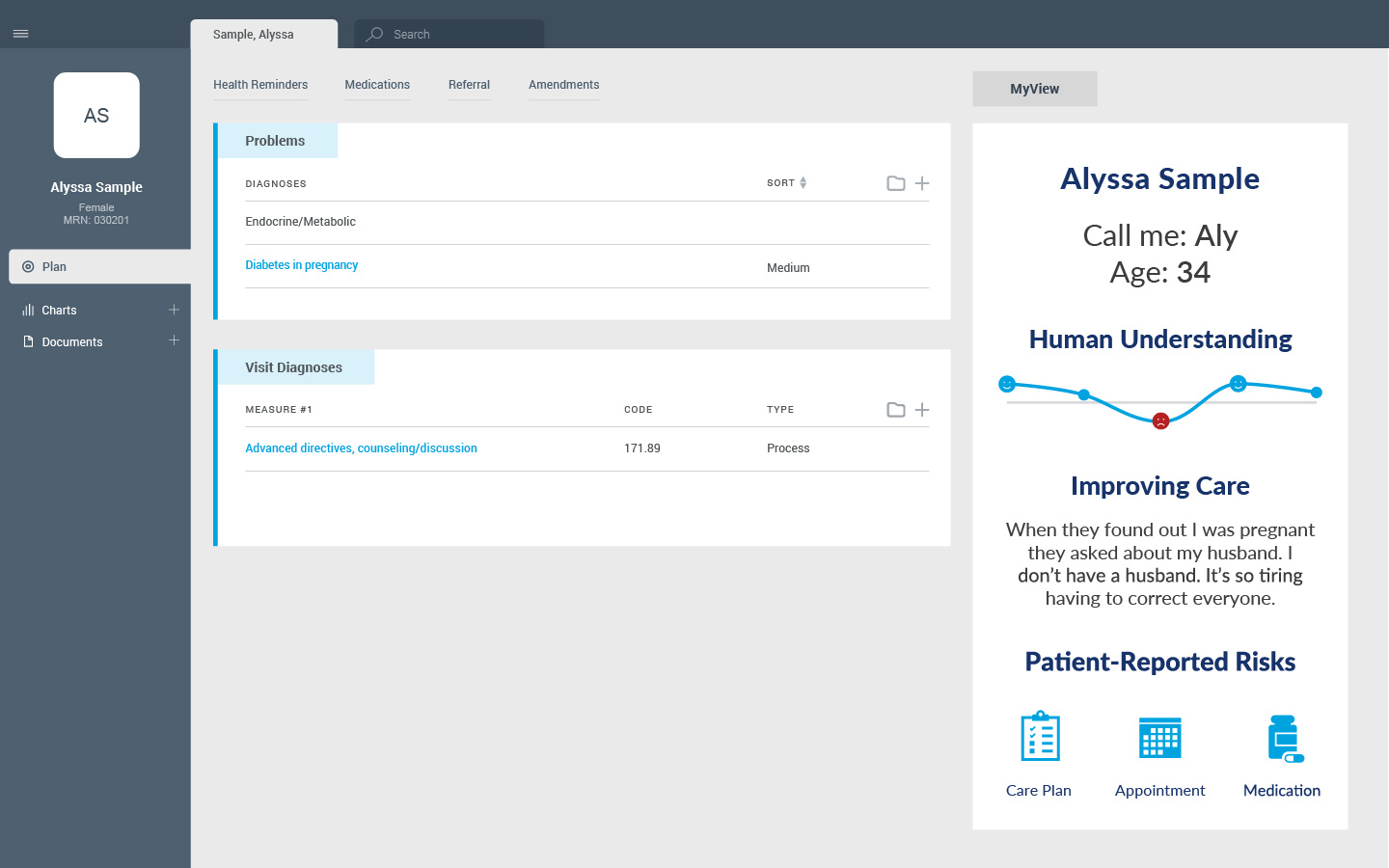
- EHR integration available for most major health systems
- Context: Patient preferences, expectations, pressures, and determinants
- Risks: Patient-reported concerns for continuing care
- Past Experiences: Key information from previous visits
- Zero clicks for care teams including office staff, nurses, physicians
- Summary review takes just 15 seconds
- Highlights new info for each care team member
Deepen your understanding with MyStory
Deepen your understanding with MyStory
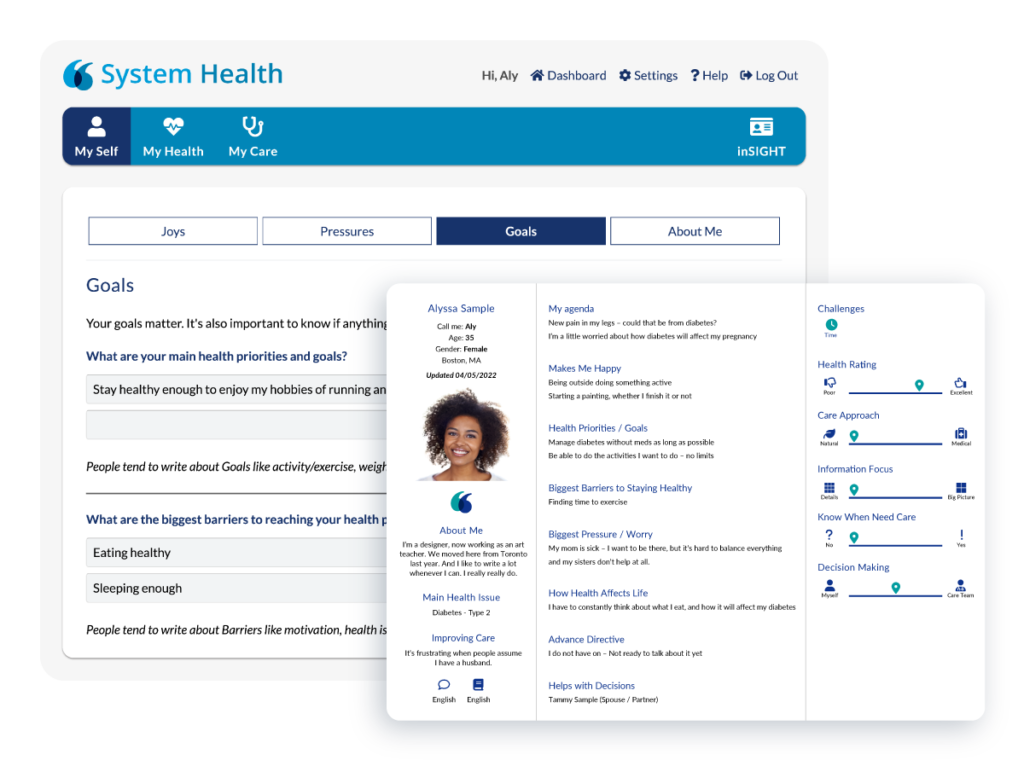
Health systems wanting a deeper understanding of the individuals they serve can implement MyStory™ and pull patient-generated contextual data into MyView. MyStory is is based on proven communication science and makes it easy for patients to share essential information that helps the care team create personalized interactions.
How it works
How it works

Patient is invited to share what matters to them via appointment reminders, e-check-ins, the patient portal, and QR codes
Preferences, goals, and expectations are summarized through NRC Health’s MyView™ and integrated into the EHR

With access to patient-driven context, care teams create a unique, personal connection

MyStory can be updated by the patient as their health needs and expectations evolve


